Medicare is a federal health insurance program for people aged 65 and older, as well as for certain younger people with disabilities. Medicare pays healthcare providers a set amount for each service or procedure they perform, with these reimbursement rates determined by the government. Over the past few decades, reimbursement rates for Medicare have been steadily decreasing. The American Medical Association has found that clinician reimbursement by Medicare has dropped by 22% from 2001 to 2021.(1) Factors such as rising healthcare costs and an aging population have led to Medicare reimbursement rates not keeping up with the actual cost of providing medical care. Falling Medicare reimbursement rates have significant impacts on the healthcare industry. When reimbursement rates fall, healthcare providers face financial challenges that can negatively impact the quality of care they provide to their patient population. Lower reimbursement rates can lead to decreased availability of care, reduced access to services, and ultimately, compromised patient outcomes. Healthcare providers also may face difficulty recruiting and retaining qualified staff, because low reimbursement rates can limit their ability to offer competitive salaries and benefits. Many providers have had to cut costs, reduce staff, or limit the services they offer in order to stay financially viable. Some providers have even stopped accepting Medicare-insured patients altogether, due to the lower rates of reimbursement, which can make it difficult for Medicare beneficiaries to find the care they need. Additionally, the decreasing reimbursement rates can discourage healthcare providers from entering certain fields or practicing in certain geographic areas, further exacerbating the healthcare access problem. Consequently, falling Medicare reimbursement rates are a serious concern for the healthcare industry and require careful attention from policymakers and healthcare leaders, and finding solutions to this issue will be crucial to ensuring that Medicare beneficiaries continue to receive the care they need. (It is possible that this outcome would be less prevalent in the field of pain management, as a large proportion of patients seeing pain management physicians are on Medicare.)
In the practice of medicine, each procedure performed and billed for by a physician is assigned a current procedural terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) code.(2) A CPT or HCPCS code is a standardized medical code used by healthcare providers to describe and bill for medical services and procedures. These codes are developed and maintained by the American Medical Association and are recognized by insurance companies, government agencies, and other third-party payers. Each code corresponds to a specific medical service or procedure, including diagnostic tests, surgeries, and other medical treatments. By using codes, healthcare providers can bill accurately for their services and ensure that they are paid appropriately for the care they provide. The value for each code is determined by relative value units (RVUs). An RVU is a measure used in healthcare to determine the value of medical services and procedures. Each medical service or procedure is assigned a specific RVU value based on factors such as the time, effort, and skill required to perform it, as well as the cost of the resources used. The total RVUs assigned to a particular service or procedure are then used to calculate the reimbursement amount that a healthcare provider will receive for that service or procedure. RVUs are updated annually by the Centers for Medicare & Medicaid Services (CMS) to reflect changes in the cost and complexity of medical services and procedures.
Although some studies have previously evaluated trends in reimbursements in other fields, a comprehensive evaluation of geographic monetary reimbursement trends in pain management anesthesia has yet to be conducted. Because these trends had not been evaluated previously, we aimed in this study to evaluate national and geographic trends of Medicare reimbursement rates in pain management anesthesia from 2000 to 2022.
Methods
For our study we selected 155 codes most frequently billed in pain management to determine trends of reimbursement rates specific to pain management anesthesia. The prices for each of these procedures were obtained from the Physician Fee Schedule Look-Up Tool from CMS. The codes were obtained by looking on the database for the American Academy of Professional Coders. Changes in Medicare reimbursement rates were calculated, averaged for each procedure, and adjusted for inflation using the consumer price index for the 23-year period.
Data and Results
Over the last 23 years, the inflation-adjusted Medicare reimbursement for the selected pain management procedures decreased annually by 2.81%. The total percentage change in reimbursement across all states and territories ranged from –17.57% to –31.69%. The map shown in Figure 1 represents the corresponding annual reimbursement trends for the appropriate state or territory.
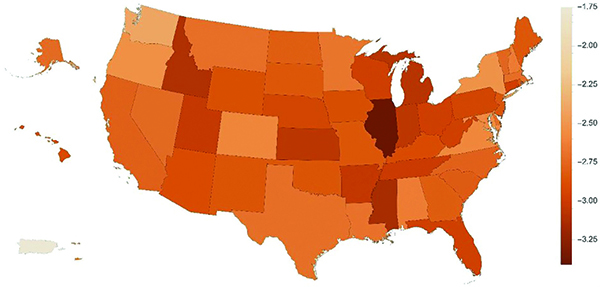
Figure 1. Changes in reimbursement for specific pain management codes 2000
to 2022.
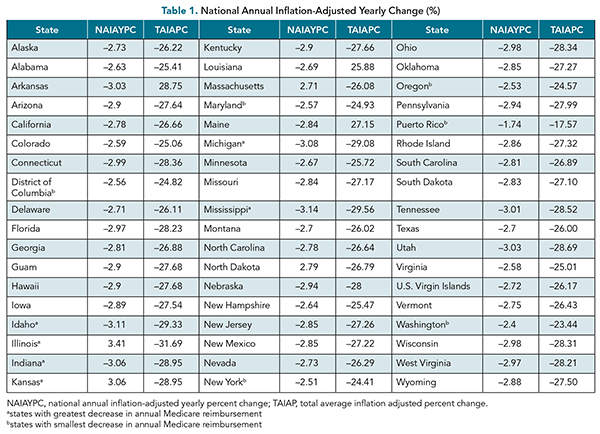
Table 1 lists every state and territory for which research was conducted, along with the national annual inflation-adjusted yearly percent change in reimbursement (NAIAYPC) and the total average inflation adjusted percent change in reimbursement (TAIAPC).
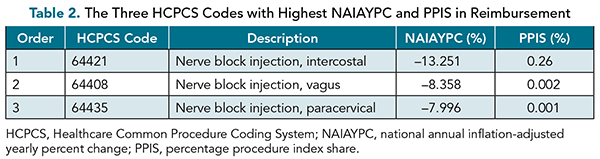
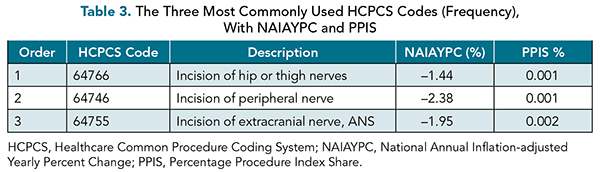
We also conducted research as to which pain management codes are billed most frequently, along with which codes showed the greatest changes in reimbursement. Table 2 illustrates the three HCPCS codes with the highest NAIAYPC, and the percentage procedure index share (PPIS) as it relates to reimbursement. Table 3 shows the top three HCPCS codes sorted by frequency, along with the NAIAYPC and the PPIS.
Discussion
Decreased Medicare reimbursement for pain management procedures is particularly concerning due to its patient population. Chronic pain is one of the most common patient presentations in a pain management clinic. The Centers for Disease Control and Prevention (CDC) estimates that 21% of adults in the United States had chronic pain in 2021 and 7% had chronic pain that results in substantial restriction of daily activities,(3) totaling almost 70 million people.
The data reveal a worrisome trend for anesthesiologists who offer pain management care to Medicare-insured patients. Currently, approximately 18.9%(4) of the population is covered by Medicare, and this number is expected to grow in the coming years due to the aging population. Reducing Medicare reimbursement rates could have adverse effects on the range of procedures accessible to patients covered by Medicare and could lead to a decline in the number of healthcare providers willing to accept Medicare-covered patients.
The discrepancies in reimbursement across different geographical locations indicate that physicians have varying incentives to practice in different areas.
The reasons for the decline in reimbursement are multifactorial, and the process of tracking the reimbursement changes is complex. As part of the Affordable Care Act, publicly available databases related to annual Medicare procedure volume, reimbursement, and hospital-related costs were created to increase transparency and reduce costs.(5) The database consists of annual procedure volume, total allowed charges, and total payments for each CPT code.(6) Analysis of the available data indicates that inflation-adjusted Medicare reimbursement for the selected pain management procedures decreased by 2.81% annually between 2000 and 2022.
Our study affirms the existence of geographical variations in reimbursement patterns. The discrepancies in reimbursement across different geographical locations indicate that physicians have varying incentives to practice in different areas, potentially resulting in future implications for patient access to pain management procedures, particularly in states with lower reimbursement rates, such as Illinois, Mississippi, and Idaho (Figure 1). We recommend further research focused on finding how decreasing rates may have potential adverse effects on physician location and relative decreases in reimbursement for pain management procedures when comparing specific locations or states.
The primary limitation of this analysis is that the insurance reimbursement data accessible to the public do not include payments from third-party payors. Although Medicare data provide insights into overall reimbursement patterns, and often are used as a reference point based on which other insurance rates are set, those data fail to consider private insurance companies that do not disclose their reimbursement data openly. Additional studies are required to assess how reducing Medicare reimbursement affects reimbursement rates from private insurance providers.
Moreover, it is important to conduct further research to understand the present and future implications of the geographical disparities in reimbursement on patient access and outcomes. Exploring new lobbying strategies for policy changes may be necessary to address the discrepancies in access and outcomes, ensuring that the quality of care for Medicare beneficiaries in areas with low reimbursement rates remains unaffected.
Conclusion
Our study examined the reimbursement trends, from the year 2000 to 2022, for the top-grossing 155 pain management procedure codes, focusing on Medicare reimbursement rates and geographical differences. Over a 23-year period, between 2000 and 2022, we found that inflation-adjusted Medicare reimbursement for the selected procedures decreased annually by 2.81%. The findings raise concerns for anesthesiologists providing pain management care to Medicare-insured patients, because lower reimbursement rates may lead to limits on procedure availability and decrease the number of providers accepting Medicare. Geographical variations in reimbursement highlight the need for further research and potential policy changes to mitigate potential access disparities and ensure quality care for Medicare beneficiaries in areas with low reimbursement rates.
References
American Medical Association. Letter to U.S. House of Representatives and U.S. Senate. AMA. December 8, 2022. https://searchlf.ama-assn.org/letter/documentDownload?uri=%2Funstructured%2Fbinary%2Fletter%2FLETTERS%2Flfdr.zip%2FAMA-State-Federation-Letter-Medicare-Cuts-Final-12-8-22-002.pdf . Accessed May 2023.
What is CPT? AAPC website. https://www.aapc.com/resources/what-is-cpt . Accessed 20 May 2023.
Rikard SM, Strahan AE, Schmit KM, Guy GP Jr. Chronic pain among adults - United States, 2019-2021. MMWR Morb Mortal Wkly Rep. 2023;72:379. https://doi.org/10.15585/mmwr.mm7215a1
Bureau UC. Health Insurance Coverage in the United States: 2021. Census.gov. www.census.gov/library/publications/2022/demo/p60-278.html . Accessed May 22, 2023
Federico V, Zavras A, Butler A, et al. Medicare reimbursement rates and utilization trends in sacroiliac joint fusion. J Am Acad Orthop Surg. 2023;31:923-930. Epub 2023 May 15. https://doi.org/10.5435/JAAOS-D-22-00800
Centers for Medicare & Medicaid Services. Part B national summary data file. www.cms.gov/data-research/statistics-trends-and-reports/part-b-national-summary-data-file . Accessed April 30, 2023.

