Medicare is a health insurance program for disabled citizens and those over the age of 64. It is federally funded, and providers offering care to Medicare beneficiaries are reimbursed for each specific service rendered. In recent decades, these predetermined rates of reimbursement have been steadily declining—by 26% in the last couple of decades.(1) Serious problems follow this decline, because reimbursement for medical care does not keep step with inflation and the rising expenses of medical treatment. Some facilities and agencies find it challenging to recruit and retain qualified staff because of weak salary and benefits offers. Some physicians may refrain from practicing certain branches of medicine or in specific geographical regions where falling reimbursement rates are most pronounced, which then worsens the difficulties with access to healthcare in those areas. The failure of Medicare reimbursements to keep pace with inflation is likely to have a significant impact on the structure and delivery of hospice and palliative care in the future.
Each service performed by the practicing professional is billed for and reimbursed according to specific standardized coding systems: Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS).(2) The codes, maintained by the American Medical Association, are recognized by insurance agencies and government committees to adequately compensate physicians for the healthcare provided. The amount reimbursed for each service is calculated using relative value units (RVUs), based on factors such as complexity or length of procedure, costs of training or equipment, and skill involved. The RVUs are regularly updated to promote the accuracy of care compensation value.
Several research projects have identified patterns in Medicare reimbursement in various areas of medical practice, but no extensive research has yet been conducted on the geographic trends of compensation for physicians practicing hospice and palliative care. This study analyzes regional patterns of Medicare reimbursement rates in hospice and palliative care from 2013 to 2022.
Method
We first identified 44 of the most frequently billed codes in palliative care from 2013 to 2022, using the database of the American Academy of Professional Coders. The Medicare reimbursement rates for each procedure for each year during the selected time period were then obtained from the Physician Fee Schedule Look-Up Tool from CMS. These national data were then stratified by census region and individual states to compare geographic trends in reimbursement rates. All metrics also were indexed against the United States Consumer Price Index (CPI) to provide inflation-adjusted changes in reimbursement rates.
Data and Results
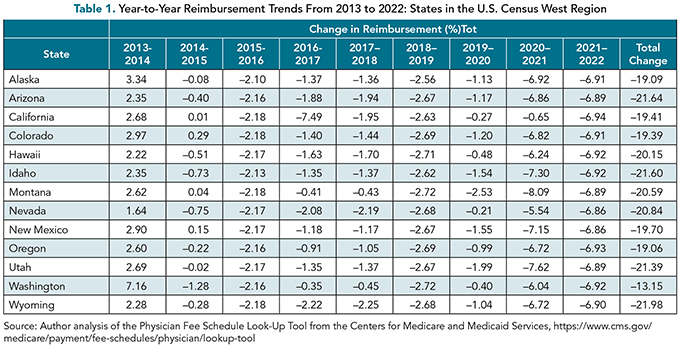
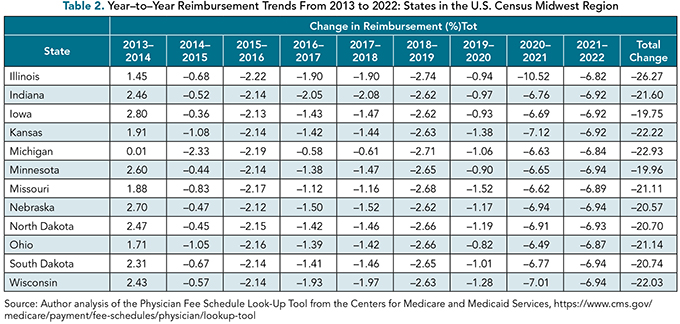
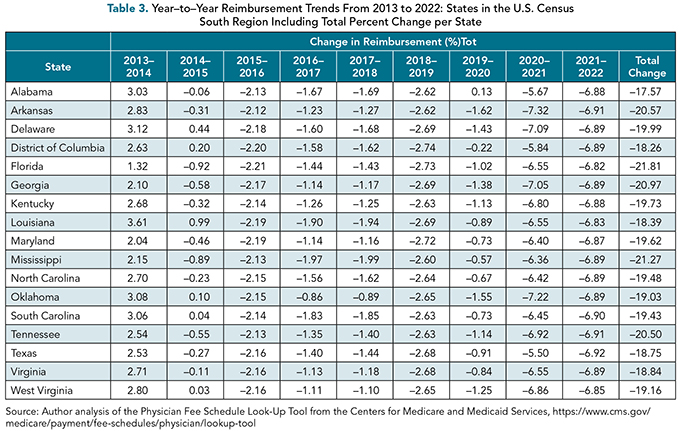
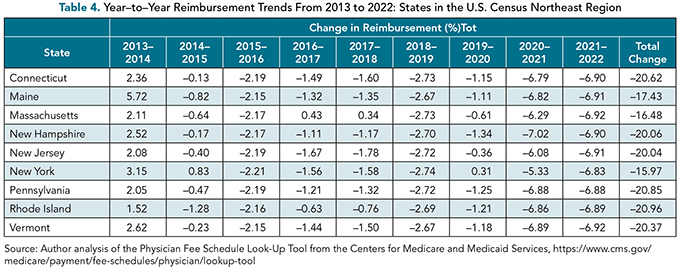
From 2013 to 2022 the inflation-adjusted Medicare reimbursement for the selected hospice and palliative medicine procedures decreased annually by an average of 2.24%. The average total reimbursement for each HCPCS procedure analyzed across that same time period fell, on average, 18.44% for all U.S. states and territories. The largest average yearly decline in reimbursement was seen in Illinois, Michigan, and Kansas, with average inflation-adjusted yearly percent changes of –2.98%, –2.58%, and –2.51%, respectively. The states and territories that showed the smallest annual decrease in reimbursement were Puerto Rico, Washington, and New York, with average inflation-adjusted yearly percent changes of –0.75%, –1.53%, and –1.82%, respectively.
Included in the analysis of the study is the inflation-adjusted year-over-year percent change in reimbursement across every U.S. state and territory from 2013 to 2022. The results are listed in Tables 1 through 4 for each state, organized by U.S. census regions. The data for additional U.S. territories are presented in Table 5.

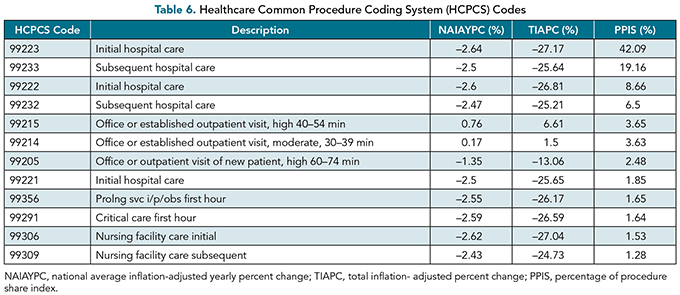
Additionally, an analysis of national trends of each of the 44 HCPCS procedure codes from 2013 to 2022 was performed. The top 12 HCPCS codes are organized by their respective shares of total revenue displayed as the percentage of procedure share index (PPIS) are presented in Table 6. These codes accounted for 94.17% of the total revenue generated among the 44 HCPCS codes analyzed and had an average total percentage change from 2013 to 2022 of –20.00%.
Discussion
From 2012 to 2021 there has been a 20.14% increase in total Medicare enrollment.(3) Of the roughly 67 million people enrolled in Medicare, nearly 1.7 million people receive hospice services each year.(4,5) These numbers are projected to increase over the next decade as our population continues to age.(6)
As part of the Budget Control Act of 2011, in order to maintain budget neutrality, Medicare payments incur a roughly 2% reduction in payout every year, known as a sequestration.(7) This originally was designed to occur annually in July from 2013 to 2021. Because of the COVID-19 pandemic and legislation that suspended payment reductions, reductions have subsequently been limited to 1%. Yearly sequestrations are now projected to continue through 2031.(8)
Yearly sequestrations, combined with our analysis of recent trends in declining reimbursement from 2013 to 2022, paint a picture of concern for the future of hospice and palliative care. The average percent change per year over this 10-year period in the HCPCS code reimbursement was –2.24%. Although this does not significantly exceed the sequestration rate required by the Budget Control Act of 2011, the average change in reimbursement when adjusted for inflation was –18.44%.
The states with the largest average yearly decline in reimbursement were Illinois, Michigan, and Kansas, with average inflation-adjusted yearly percent changes of –2.98%, –2.58%, and –2.51%, respectively. This gives these states a total percent change of –26.27% (Illinois), –22.93% (Michigan), and -22.22% (Kansas).
We also have gathered data on the most frequently used codes in hospice and palliative care. Of the 44 HCPCS codes analyzed, 12 account for 94.17% of the total revenue generated. On average, each of these codes saw roughly a 20% decline in reimbursement over the time period analyzed.
The American Hospital Association revealed that hospitals experienced a –8.5% margin in 2020 and at that time were expected to experience a –9% margin in 2022 when being paid by Medicare. Approximately 94% of hospitals have half of their inpatient costs paid by Medicare or Medicaid. With the accelerated reduction in reimbursement, hospitals are forced to raise prices to compensate, potentially limiting access to care due to financial restrictions.(9)
Conclusion
This article examines Medicare reimbursement trends in 44 of the most frequently billed HCPCS codes in hospice and palliative care from 2013 to 2022. Over that 10-year period, there was an average annual percent change of –2.24% and an average total change per state of –8.44%. The three states or territories with the largest decrease in reimbursement over this time period were Illinois, Michigan, and Kansas; the three states or territories with the smallest decrease in reimbursement were Puerto Rico, Washington, and New York. Although the average annual percent change is not drastically higher than the sequestration rate required by the Budget Control Act of 2011, the length of time these sequestrations could be in effect has the potential to drastically reduce reimbursement for hospice and palliative care doctors, and, therefore, limit patient access to care. We recommend additional studies be done to explore how policies, legislation, and other means may mitigate the risk these sequestrations have on the field of hospice and palliative care.
References
American Medical Association. The need for Medicare physician payment reform. 2023. AMA. www.ama-assn.org/system/files/ama-medicare-reform-grassroots-insert.pdf
What is CPT? AAPC.com. www.aapc.com/resources/medical-coding/cpt.aspx . Accessed May 20, 2023.
CCW t counts, 2012–2021. CMS Chronic Conditions Data Warehouse. Table A.1.A. Medicare Beneficiary. www2.ccwdata.org/documents/10280/19096644/ccw-website-table-a1a.pdf
AAMC. Hospice and palliative medicine. Careers in Medicine. https://careersinmedicine.aamc.org/explore-options/specialty-profiles/hospice-and-palliative-medicine#overview
U.S. HHS Office of Inspector General . Hospice. April 1, 2023. HHS. https://oig.hhs.gov/reports-and-publications/featured-topics/hospice/#:~:text=It%20may%20be%20provided%20in,billion%20annually%20for%20this%20care
Caplan Z, Rabe M. The older population: 2020. 2020 Census Briefs. May 2023. www2.census.gov/library/publications/decennial/2020/census-briefs/c2020br-07.pdf
Fact sheet: Medicare sequester relief extension needed for health providers: AHA. American Hospital Association. September 2022. www.aha.org/fact-sheets/2022-09-13-fact-sheet-medicare-sequester-relief-extension-needed-health-providers
Congressional Research Service. Medicare and budget sequestration—CRS reports. March 29, 2022. https://crsreports.congress.gov/product/pdf/R/R45106
Fact sheet: Majority of hospital payments dependent on Medicare or Medicaid: AHA. American Hospital Association. May 2022a. www.aha.org/fact-sheets/2022-05-25-fact-sheet-majority-hospital-payments-dependent-medicare-or-medicaid

