Summary:
Trends are not expected to return to prerecession growth rates, although there are certain career paths providing greater opportunities for increased earnings.
Trends are not expected to return to prerecession growth rates, although there are certain career paths providing greater opportunities for increased earnings.
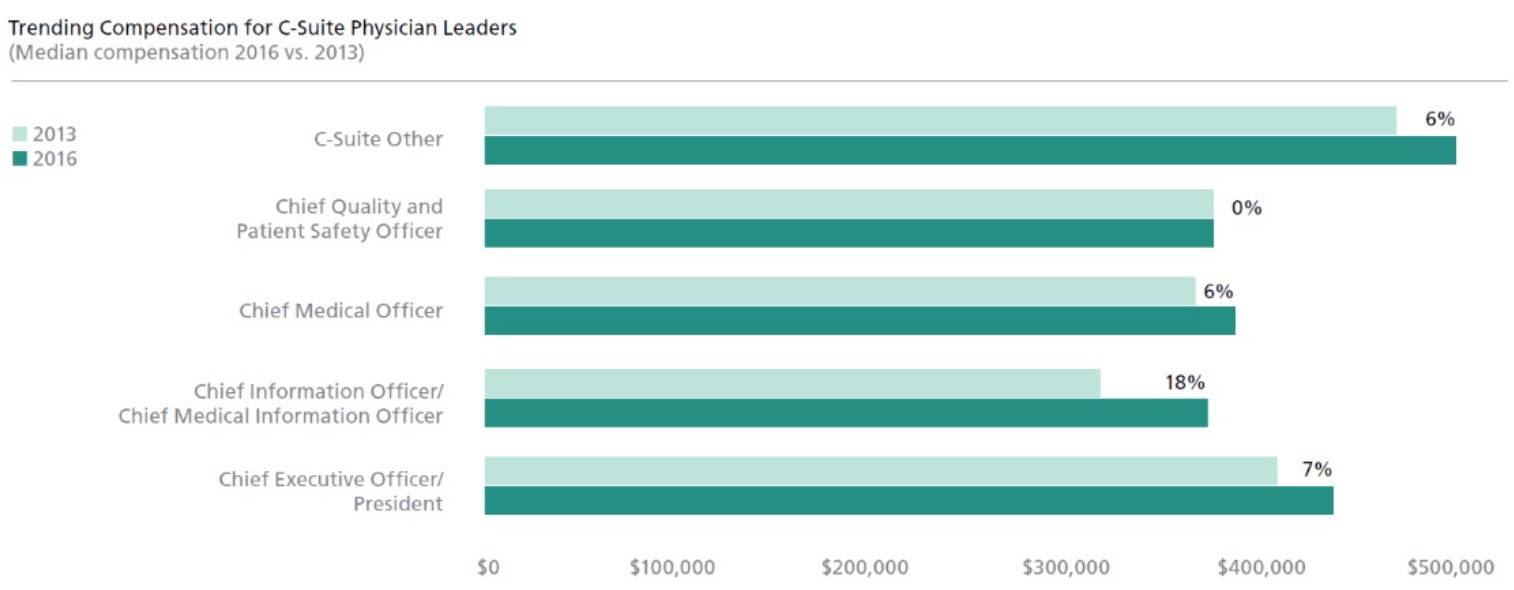
Total median compensation for physician leaders in 2016 reached $350,000, a two-year increase of 8 percent from $325,000 reported in 2013, according to results of this year’s Physician Leadership Compensation Survey by Cejka Executive Search and the American Association for Physician Leadership.
The survey was completed by 2,353 respondents and, although compensation trends have been fairly consistent over the past seven years, they are not expected to return to prerecession growth rates of 12 percent reported in 2007 — given health care reform and the continued scrutiny on costs, including executive compensation.
Pathways to Higher Compensation
However, there are certain career paths providing physician leaders with greater opportunities for compensation growth. For example, those working at the corporate or parent-level of a health system saw a 22 percent spike in median compensation since 2013. Physician leaders holding a master’s in business administration on average earned 7 percent more than those without an MBA. In addition, leaders who allocated more time to administration and whose performance-based pay was a higher percentage of total compensation, earned more as well.
CEO Not Always the Highest Paid
Surprisingly, the highest paying 2016 position at $499,000 is “C-Suite-Other,” suggesting that chief executive officer may not always be the top job at health care organizations. This category comprises roles such as physician in chief, chief strategy officer, chief transformational officer, chief innovation officer, chief clinical officer and chief integration officer.
Many of these roles have been formed in response to a greater number of more complex initiatives hospitals and health systems must tackle to keep pace with the move toward population health management and accountable care. Physicians in these transformative roles often are tasked with “connecting the dots” across the organization and care continuum to achieve the greater efficiency and effectiveness of care required by newer reimbursement models.
Big Data Drives Compensation Higher
However, the greatest increase in C-suite compensation since 2013 was 18 percent for physicians in the chief information officer/chief medical information officer roles. Previously focused on electronic medical records implementation, information and medical information officers today often are jointly responsible with chief quality and patient safety officers for ensuring the usability of data to support preventive care at the individual provider level and risk-based accountable care at the enterprise level. Clearly, there is perceived value in having a physician leader drive these initiatives and facilities are willing to compensate accordingly.
Demand for Clinical Quality Leaders Remains Strong
This follows with a trend we observed in median compensation for the chief quality and patient safety officer role, which spiked 22 percent from 2011 to 2013, in response to the anticipated effects of the Affordable Care Act signed by President Barack Obama in 2010. As CIO compensation caught up, chief quality and patient safety officer compensation in 2016 remained flat with 2013.
The highest two-year pay gain outside of the C-suite was 26 percent for physician leaders focused on clinical initiatives, such as president of the medical staff and medical director, assistant or associate. The number of respondents in these positions also rose as a percentage of total physician leaders, from 5 percent in 2013 to 8 percent in 2016, indicating an emphasis on building the next organizational level of quality leaders in response to health care reform, which now significantly ties reimbursements to quality outcome measurements.
Does It Pay to Be in Administration?
According to the survey, the answer is yes. The majority of respondents devote more than half of their time to administrative duties. Median compensation for those who spend 25 percent or less of their time in administration is $50,000 compared to $360,000 for those who allocated 100 percent of their time to administration. In addition, the majority (51 percent) of physician leaders report that by compensating them for administrative time, their organizations “make them whole” for time lost from clinical productivity.
In terms of administrative tenure, physicians received the highest jump in median compensation at the three- to five-year mark (4.3 percent). Meanwhile, the majority of physicians (58 percent) have been in a paid administrative job for more than 10 years.
Although physician leaders as a whole devote less time on administration than in 2013 (62 percent vs. 68 percent), in those who reported spending the highest percentage of time on administrative duties are: chief quality/patient safety officers (88 percent), medical affairs executives (88 percent) and CMOs (87 percent).
More Strategic Influence
Not surprisingly, those who allocated the greatest percentage of their time to clinical duties were presidents of medical staff (61 percent), medical directors and service line leaders (56 percent) and assistant and associate professors (54 percent). For all physician leaders, the greatest portion of their administrative time (18 percent) is spent on “performance,” which includes oversight of quality, efficiency, clinical effectiveness, patient satisfaction or financial benchmarks and outcomes, execution of best practices, process improvement and problem resolution/remediation. The second is “medical management” (16 percent), which includes clinical advisory, protocols, guidelines and services, population health and disease management, development of new care models, quality/risk management and peer review.
Post-Grad Degrees a Path to Higher Compensation
Median compensation for all physician leaders holding a post-graduate degree is $354,167, 5 percent higher than those without a post-graduate degree.
Among C-level executives:
CEOs holding an MBA reported 13 percent higher median compensation.
CEOs holding an MBA ($450,000) earned 8 percent more than those with an MMM ($415,000).
CMOs holding an MBA ($400,000) earned 11 percent more than those who do not ($360,000).
CMOs holding an MMM ($430,000) earned 19 percent more than those who do not ($360,000), and 8 percent more than those with an MBA.
CMOs holding an MPH ($389,000) earned 8 percent more than those who do not ($360,000).
CMOs holding a CPE ($376,400) earned 5 percent more than those who do not ($360,000).
Medical affairs executives holding a CPE ($407,500) earned 20 percent more than those who do not ($340,000).
Of all of the survey respondents, 40 percent hold at least one post-graduate degree or certification:
51 percent master of business administration (MBA).
23 percent certified physician executive (CPE).
17 percent master of medical management (MMM).
14 percent master of public health (MPH).
7 percent master of health administration (MHA).
Given the expanding scope of responsibilities and perspective required of leadership roles in a post-reform era, there is anecdotal evidence that suggests post-graduate degrees will become more prevalent for physician leaders in the future.
Performance-Based Pay Leads to Higher Compensation
Physician leaders with a greater percentage of compensation at risk or, based on bonus, report higher median compensation. These physicians also experienced a higher rate of increase in median compensation since 2013.
For the first time since it was measured in 2003, personal goals (51 percent) have tipped the scale, exceeding organizational goals (49 percent) in determining incentive-based compensation. This is a shift from 2013 (56 percent organizational and 44 percent personal), as board members seek to effectively incentivize physician leaders operating in a challenging environment in which results may not be realized for several years.
Accordingly, the two most commonly mentioned bonus components in 2016 are clinical quality (52 percent), which includes measurements, outcomes, safety and process; and financial performance (51 percent), which includes cost-containment and organization profit.
Roles of Physician Leaders More Influential and Complex
One of the overarching trends we have observed in all health care senior management is the need to manage people and outcomes through influence, rather than direct authority. The primary factors are the comprehensive, interdependent and urgent nature of transformation initiatives, which requires collaboration and engagement among a broad base of stakeholders in order to succeed. Physician leaders offer unique perspectives and credibility that can enhance engagement levels among clinical and non-clinical constituents alike. In an effort to maximize their value, physician leaders today operate in an increasingly complex environment. More than half (54 percent) have multiple or shared administrative reporting relationships, up from 50 percent in 2013. Of those, 49 percent (versus 24 percent in 2013) are administratively accountable to more than one person, and 29 percent (versus 19 percent in 2013) have shared direct reports. In addition, 22 percent are a dyad partner, which requires heightened levels of collaboration, communication and trust to achieve mutual performance objectives and goals.
As a result, physician leaders report increasing levels of influence within their organizations. A large portion (45 percent) are part of the executive management team reporting directly to the CEO/president. A majority (66 percent) of physician leaders in the CEO/president role are members of the board of directors, but also a significant percentage (21 percent) of C-suite others, as well as 20 percent academic department chairs/division chiefs, 20 percent consultants, full-time and 19 percent chief quality/patient safety officers. Perhaps most noteworthy is that, regardless of formal stature, an impressive number of physician leaders (61 percent) say they have more strategic influence this year, as compared to the prior year.
The findings show that physician leaders as a whole are enjoying greater compensation, influence and scope of responsibility, underscoring the vital role they play in shaping health care delivery for years to come.
Paul Esselman is senior executive vice president and managing director at Cejka Executive Search in St. Louis, Missouri.
The 2016 Physician Leadership Compensation Survey can be ordered online at cejkaexecutivesearch.com .
Topics
Economics
Related
The Collaboration Imperative: Why Healthcare Executives Must Unite Against an Existential ThreatWhy Big Companies Struggle to Negotiate Great DealsMedPac Finds the Hospital Industry is on a More Stable Financial Footing Now

